Wound management 1 – Emergency management of open fractures
Written by James Roush
An open fracture is any fractured bone that is exposed to environmental contamination due to disruption of soft tissues surrounding the bone. By extension, if there is a skin wound in a limb or body segment that has a fracture...
Key Points
Any fracture with a skin wound anywhere in that body segment should be considered an open fracture and to be at increased risk for later infection.
Open fracture wounds should be treated on an emergency basis, but immediate rigid stabilization of the fracture itself is not an emergency.
Every patient with vehicular trauma should receive a minimum of chest and abdominal radiographs, CBC, serum chemistry, ECG, pulse oximetry and blood pressure measurements to assess potential co-morbidities.
Initial sterile wound dressings should be applied while the patient is assessed and stabilized to protect against infections from nosocomial organisms, and systemic broad-spectrum antimicrobials should be given as soon as possible.
External skeletal fixators allow open wound access while providing rigid fixation, preserving bone blood supply and minimizing soft tissue disruption.
Introduction
An open fracture is any fractured bone that is exposed to environmental contamination due to disruption of soft tissues surrounding the bone. By extension, if there is a skin wound in a limb or body segment that has a fracture, this should be considered as an open fracture, regardless of whether or not the fracture is assumed to communicate with the wound. One study reported that open fractures occurred in 16.7% of all traumatic fractures in dogs and cats, and vehicular trauma, younger age, larger body weight, and fracture comminution were associated with a greater likelihood of open fracture [1].
Proper treatment of open fractures requires recognition of two central facts:
- The degree of future morbidity resulting from open fracture repairs is often directly related to the initial emergency management of the fracture.
- Open fractures present unique management challenges to the practicing surgeon in terms of additional considerations for fracture repair and in wound care and closure.
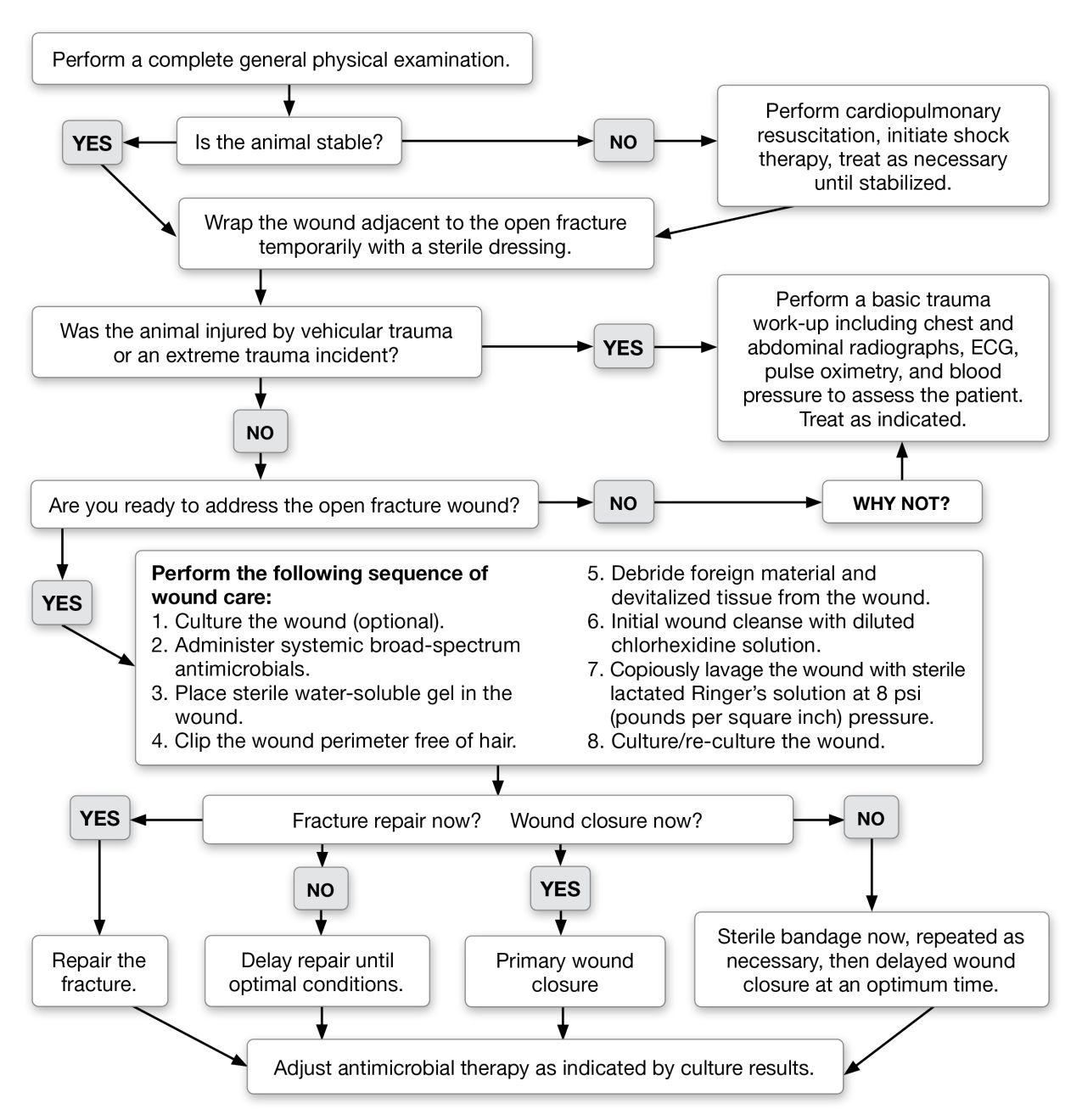
Open fractures are often the results of vehicular trauma or other high-energy events, and such trauma can result in significant co-morbidity that must be addressed. In addition to limiting future morbidity, initial management of patients with open fractures is critically important to minimizing cost and healing time, and to the functional outcome of the patient. Especially when treating open fractures, veterinarians are best advised to strictly adhere to established principles and not attempt to cut corners to save time, cost or effort. Post-operative osteomyelitis or non-union nearly always results from compromises made in initial wound and fracture care. Figure 1 provides a useful algorithm for management of patients with open fractures.
Patient assessment
Open fractures should always be appropriately treated on an emergency basis, but the fractured bone itself does not need emergency repair. Certainly, recognition of the open nature of a fracture does not supersede the care of more life-threatening injuries or co-morbidities. The first and most important action in open fracture diagnosis and management is to thoroughly assess the patient for additional systemic abnormalities. All animals with open fractures due to trauma should be assessed for occult injuries to the thorax and abdomen, and should have a complete neurologic examination in order to rule out pre-existing neurologic dysfunction or additional neurologic injury. One study reported that 57% of dogs with skeletal injury had radiographic, electrocardiographic, or other evidence of thoracic trauma, including pulmonary contusion, myocardial contusion, pneumothorax, or diaphragmatic hernia [2]; however, only 21% of the dogs had associated clinical signs of thoracic injury. Every animal sustaining vehicular or other trauma sufficient to result in long bone fracture should receive a minimum database of routine chest and abdominal radiographs, complete blood count (CBC), serum chemistry, blood pressure assessment, pulse oximetry and a diagnostic electrocardiogram (ECG). Post-traumatic cardiac arrhythmias may not appear for 48-72 hours after the event, so ECG’s that are initially normal should be repeated at 12-hour intervals for 72 hours post-trauma. Patients with initial or subsequent cardiac arrhythmias, or with other systemic trauma, should be treated appropriately for any life-threatening injuries, and fracture repair delayed until the physical condition stabilizes. The neurologic status of each animal must be assessed to rule out central nervous system injuries and peripheral fracture-associated injuries. Urologic injuries are common in patients with pelvic or femoral fractures, and may result in hyperkalemia and uremia before the injury is detected. Urine output should be carefully monitored, especially in recumbent animals.Initial open fracture management
Two factors are considered paramount in proper initial management of the fracture itself. The first is the “grade” of the fracture. Open fractures in veterinary patients are commonly classified from Grades I through III (Table 1) in an effort to better predict any potential for increased morbidity or post-operative infection, but evidence for the efficacy of grading open fractures in veterinary medicine is scant. Grade I open fractures in the past have been erroneously described in the veterinary literature as fractures where the bone “penetrated from within”, a distinction that implies a pattern of displacement during trauma that cannot be determined simply by viewing the fracture and wound after injury. This assumption of the sequence of trauma should be avoided by veterinarians and in future veterinary literature. Some authors subdivide Grade III open fractures into three subtypes [3], but subclassification for management purposes is not supported by improved fracture outcomes in the available literature.
| Grade I | An open fracture with an associated wound < 1 cm in diameter. Grade I fractures are often simple, two-piece fractures and are associated with minimal soft tissue trauma. |
| Grade II | An open fracture with a skin wound > 1 cm diameter but without extensive soft tissue trauma or comminution. |
| Grade III | An extensively comminuted open fracture with severe soft tissue trauma and a skin wound of > 1 cm diameter. All fractures caused by projectiles are considered Grade III. |
The second and more important factor in open fracture management is consideration of the nature and duration of the microbial contamination, with a “golden period” for wound closure often described as being a period of 6 to as long as 12 hours from the initial wound trauma. In reality, the “golden period” is not strictly limited to duration, but is more appropriately viewed as the perceived degree of wound contamination or infection that has occurred up to the time of debridement and closure. Within the first 6-12 hours, contaminated wounds, including wounds that communicate with fractures, may be converted to clean wounds by effective surgical debridement and lavage, and then closed in primary fashion, decreasing the time to complete wound healing and wound care costs. After 12 hours, most wounds, regardless of any assumption concerning the degree of contamination, should be similarly debrided and lavaged, but should be closed over surgical drains or left open for delayed closure techniques. Decisions regarding wound closure or non-closure should be ideally based on peri-operative examination of a Gram-stained smear of the wound taken before debridement or lavage. The presence of visible bacteria in the smear indicates likely infection of > 1X105 bacteria/mm2 in the wound and therefore a recommendation that the wound should be managed as an open wound until uncomplicated healing with delayed closure techniques is likely to be achieved.
For all patients, a temporary sterile bandage or dressing should be placed over the wound as soon as possible during initial assessment of the patient. Ideally, samples for aerobic and anaerobic culture are collected at the level of the fractured bone at the time of presentation, although a prospective, randomized study found that only 18% of open fracture infections were caused by organisms found on initial culture [4]. In a study of bacterial contamination in 110 canine fractures, 72.7% of dogs with open fractures had a positive culture for aerobic and/or anaerobic micro-organisms [5]. Appropriate doses of broad-spectrum antimicrobials (see below) should be given systemically immediately after wound culture. During wound care, the animal should be placed in an aseptic environment such as a surgical suite, and all personnel should follow aseptic protocols to minimize iatrogenic contamination. Regardless of the assessed open fracture grade, and as soon as the patient is otherwise determined to be systemically stable, the open wound should be clipped free of hair to a wide margin, cleaned of gross debris by surgical antiseptic soaps, and all damaged or necrotic soft tissue debrided (Figure 2). To decrease iatrogenic contamination of the wound, the wound can be filled with sterile, water-soluble lubricant prior to clipping. Isolated bone fragments without soft tissue attachments should be removed. After debridement an initial cleansing with diluted chlorhexidine gluconate solution is recommended [3].

Debrided and cleansed wounds should then be copiously lavaged with sterile lactated Ringer’s solution or similar sterile isotonic solution; lavage volumes of 3-5 liters of isotonic solution in a 1 cm diameter wound are not excessive. It is important that lavage is achieved by a pressure of 7-8 psi (pounds per square inch) to assure adequate disruption of bacterial adherence from the tissue while causing minimal damage to healthy tissues adjacent to the wound; this is achievable with either a commercial surgical lavage device or by using a 19 G needle placed on a 60 cc syringe and vigorously sprayed over the wound. These methods assure a fluid pressure of approximately 8 psi, which is the strength of bacterial adherence to the wound surfaces. Higher pressure lavage is detrimental to healthy tissue and is not recommended. The use of antibiotics or antiseptic compounds in the lavage solution is not necessary and may be detrimental to the normal cellular elements of the tissue, but a solution of 0.05% chlorhexidine has been determined to provide antibacterial activity without causing tissue reaction [6].
Cleansing, debridement, and lavage should include the entire depth of the wound down to the fracture. Following copious lavage, the wound should again be aerobically and anaerobically cultured to assess and properly treat the microbial population left in the wound at the time of closure. At this stage the clinician should assess the tissue viability and degree of contamination and choose one of three options; repair the wound by primary means; repair the wound using a closed, sterilely maintained surgical drain; or manage the open wound with sterile dressing materials until closure can be performed at a later date, or until secondary intention healing occurs.
Broad-spectrum antimicrobial therapy
Temporary and definitive fracture stabilization
Open fractures do not require definitive stabilization immediately if proper emergency wound care has occurred. Definitive rigid fracture stabilization should only occur when the patient is appropriately stabilized, an experienced surgeon is to hand, and with all anticipated fixation devices and equipment immediately available.
Temporary stabilization of open fractures is performed to increase patient comfort and to minimize local soft tissue swelling and further soft tissue injury. Fractures of the lower extremities have less soft tissue coverage, and closed fractures may become open fractures or undergo additional comminution if unsupported. Analgesics (preferably opioid agonists such as morphine) should be administered to the patient to improve comfort.
Fractures proximal to the elbow or stifle are difficult to stabilize with external coaptation alone, and the patient should be cage-confined without splinting and treated with analgesics until definitive repair. Fractures distal to the elbow or stifle should be stabilized with external coaptation until definitive fixation or while awaiting transport to a referral center. External coaptation should consist of either a Robert-Jones bandage, or a modified Robert-Jones incorporating a molded lateral fiberglass splint. For fractures with wounds left open after debridement, all bandage materials should be sterile and applied in aseptic fashion. External coaptation should always immobilize the joint immediately proximal to the fracture and extend distally to the toes.
Definitive open fracture repair
- On careful pre-operative planning, including assessment of the fracture on orthogonal radiographs or by computed tomography
- On local availability of the surgical expertise, experience and equipment indicated for the particular fracture
- On individual patient considerations such as temperament, patient confinement opportunities, and likely owner compliance
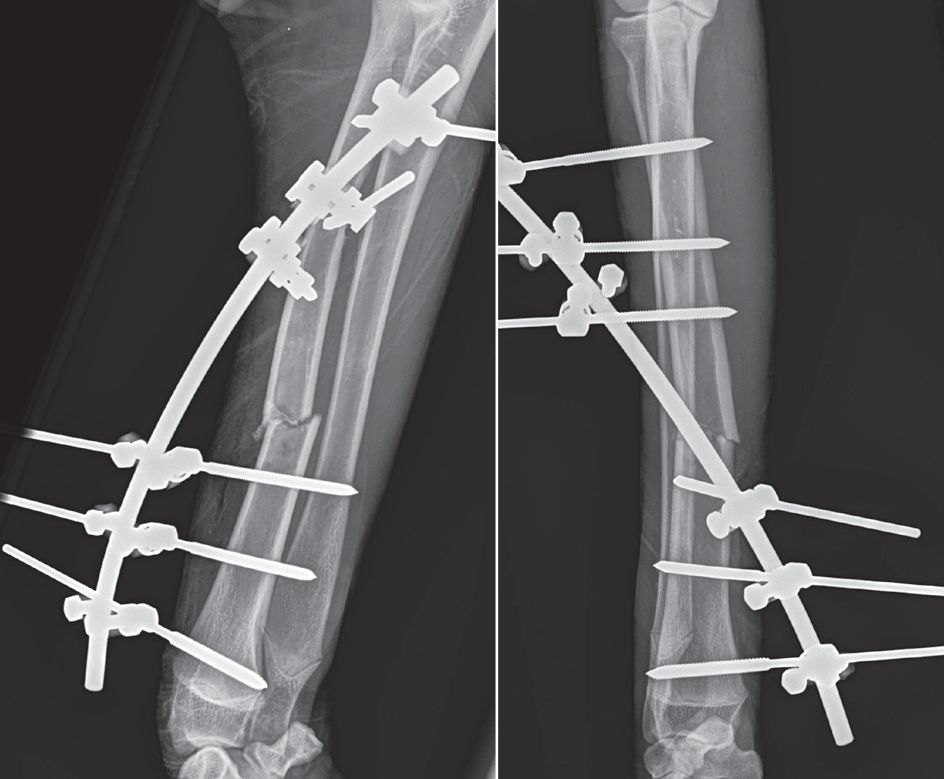
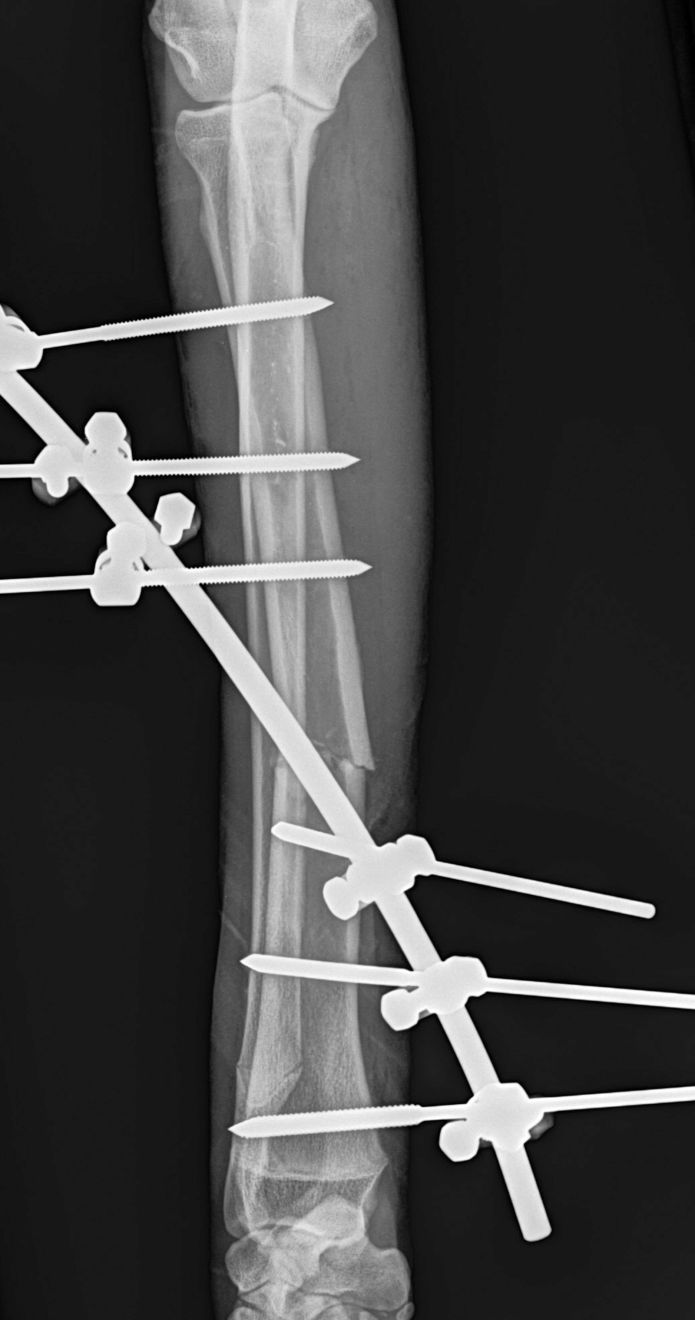
Other unique considerations for the repair of open fractures, in addition to the timing of initial wound cleansing or definitive surgical intervention, are determined primarily by the continued presence of an open wound that requires care. Fractures with wounds that are to be managed in open fashion are particularly amenable to fixation by rigid or circular ring external skeletal fixators because these devices allow frequent bandaging, debridement, lavage and daily wound care without disruption of the fixation, and because the “closed” placement of such devices minimizes further soft tissue trauma and maximizes bone viability (Figure 3a and b). Surgeons should not, however, necessarily eliminate bone plating as an option in fractures with open wounds, but if bone plates are applied and exposed to the open wound, the surgeon should anticipate a need to remove the plate after the fracture has healed as it will serve as a nidus for future infection. Bone plates may, in extreme circumstances such as extensive loss of soft tissues over the bone, be left exposed so that the wound and soft tissues may granulate over the plate during healing. Fractured bone will heal in the presence of contamination or infection if the fracture repair remains rigidly stable, and thus bone infection is not a cause for immediate repair revisions. If bone fragments have been debrided and the fracture gap requires a bone graft, delayed autogenous bone grafting is recommended approximately two weeks after wound closure or after existing infections have cleared.

Conclusion
Potential complications for open fractures include superficial wound infection, wound dehiscence, acute or chronic osteomyelitis, and delayed union or non-union. Despite a literature search for retrospective or prospective studies of infection rates in dogs with open fractures, the author could not find a report of a large case series within the past two decades. Large, broad case series infection rates after open fractures in people are also not often reported today in lieu of smaller geographically- or bone-specific reports, however a review of infection rates after open tibial fracture in people in the last decade listed infection rates between 0-25% [8], and a recent retrospective study of 296 open radius or ulna fractures had an overall incidence of deep infection of 5% [9]. Careful and sterile wound cleansing, debridement, copious lavage, administration of early broad-spectrum antimicrobials, and rigid fracture stabilization are best practices to decrease the incidence of complications in open fractures.
References
- Millard RP, Weng HY. Proportion of and risk factors of the appendicular skeleton in dogs and cats. J Am Vet Med Assoc 2014;245:663-668.
- Selcer BA, Buttrick M, Barstad R, et al. The incidence of thoracic trauma in dogs with skeletal injury. J Small Anim Pract 1987;28:21-27.
- Millard RP, Towle HA. Open fractures. In: Tobias KM, Johnston SA, eds. Veterinary Surgery: Small Animal (1st ed) St Louis: Elsevier, 2012:572-575.
- Patzakis MJ, Bains RS, Lee J, et al. Prospective, randomized, double-blind study comparing single-agent antibiotic therapy, ciprofloxacin, to combination antibiotic therapy in open fracture wounds. J Orthop Trauma 2000;14:529.
- Stevenson S, Olmstead ML, Kowalski J. Bacterial culturing for prediction of postoperative complications following open fracture repair in small animals. Vet Surg 1986;15:99-102.
- Lozier S, Pope E, Berg J. Effects of four preparations of 0.05% chlorhexidine diacetate on wound healing in dogs. Vet Surg 1992;21:107-112.
- Leonidou A, Kiraly Z, Gality H, et al. The effect of the timing of antibiotics and surgical treatment on infection rates in open long-bone fractures: a 6-year prospective study after a change in policy. Strategies Trauma Limb Reconstr 2014;9:167-171.
- Ktistakis I, Giannoudi M, Giannoudis PV. Infection rates after open tibial fractures: are they decreasing? Injury 2014;45:1025-1027.
- Zumsteg JW, Molina CS, Lee DH, et al. Factors influencing infection rates after open fractures of the radius and/or ulna. J Hand Surg Am 2014;39:956-961.
James Roush
DVM, MS, Dip. ACVS
United States
Dr. Roush is a Diplomate of the American College of Veterinary Surgeons and is currently the Doughman Professor of Surgery at the College of Veterinary Medicine, Kansas State University. Dr. Roush has authored or co-authored over 150 refereed papers, abstracts, summary articles, and book chapters on small animal orthopedic surgery, and lectures frequently at national and international meetings on fracture repair. He has over 30 years’ experience in veterinary orthopedic and neurologic surgery, orthopedic research, and small animal orthopedic surgical training of residents and students.
Other articles in this issue
Share on social media